An Air Pocket Glove for Finger Rehabilitation and Quantitative Assessment of Hemiplegic Patients
1School of Mechanical and Control Engineering, Handong Global UniversityCopyright © The Korean Society for Precision Engineering
This is an Open-Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
This paper proposes an air pocket glove for finger rehabilitation and diagnosis of hemiplegic patients after stroke. This device consists of pneumatic actuators that expand when air is injected from a pump motor, silicone flexors that act as artificial finger tendons, film-type bending sensors, and a pressure sensor. As air enters the glove, the actuators are expanded, thus stretching out paralyzed fingers. We designed two different rehabilitation modes: continuous passive motion (CPM) mode and master-slave mode, where the motions of the unaffected fingers are duplicated in the affected fingers. We conducted an experiment to test the validity of the device for each mode. In CPM mode, the patient's spasticity level was estimated from finger angle and air pressure. Our results showed that spasticity level decreased 13% from the initial level after rehabilitation. With the master-slave mode, EMG signals were additionally measured and compared to those found during conventional therapy, which revealed a positive effect stemming from voluntary involvement in the exercise. As a result, EMG energy was shown to increase up to 18% during master-slave mode.
Keywords:
Hemiplegia, Finger rehabilitation, Air pocket-type actuator, Spasticity, Assessment, Electromyography키워드:
편마비, 손가락 재활, 공기팽창형 액추에이터, 경직, 평가, 근전도 검사1. Introduction
70% of hemiplegic stroke patients suffer from upper limb impairment, and upper limb rehabilitation is closely related to ADL function recovery.1,2 Among other body parts, hands are densely packed with joints and nerves, making the most diverse and delicate movements.3 Finger rehabilitation of hemiplegic patients is practiced to relax stiffened fingers to increase function and ultimately to perform daily life behaviors.
Many finger rehabilitation exercises and diagnosis standards have been proposed as the necessity of finger rehabilitation was proved through various clinical studies. Patients who participated in Activity Card Sort (ACS) rehabilitation improved their leisure activity participation level in Functional Independence Measure (FIM) evaluation4,5, and rehabilitation through the Box and Block Test (BBT) increased the finger dexterity and affected overall upper extremity function.6,7 Furthermore, hemiplegic patients after finger rehabilitation showed higher independence and their Reintegration to Normal Living Index (RNLI) results represented positive satisfaction with life.8,9 In addition to traditional occupational therapy, end-effector and exoskeleton devices have been developed for finger rehabilitation, and they are capable of high-dosage and high-intensity rehabilitation.10 Patients who were rehabilitated with physical therapy and rehabilitation orthosis showed higher functional restoration efficiency than rehabilitation only with physical therapy.11-13
However, existing rehabilitation methods (occupational or physical therapies) are mostly simple repetitive exercises. In this case, it weakens the patient’s concentration. In addition, it is difficult to induce patient’s participation because it does not include patient’s intent and motivation during the exercise.14 In robotic rehabilitation, the movement of the orthosis is implemented along the direction of muscle contraction (flexion). But in actual rehabilitation field, exercises are performed toward extension motions because to relax muscles and joint spasticity.15,16 At last, the components of the traditional devices are developed based on the rigid body, and include a linkage that acts as rotation joint of finger. Linkage has a complicated structure that makes it difficult to match the finger joints with the device joints, and it is difficult to conduct independent rehabilitation due to the material limitations.17
In this study, we propose an air pocket glove to assist the finger rehabilitation of stroke patients with limited finger movement. air pocket glove is a wearable- type that easy to don and doff, and soft finger movements are implemented using air pocket-type soft actuator with biomimetic technology. It also behaves in an extension direction similar to actual rehabilitation, allowing grip and release, and flexible operation.
This device has two modes for effective rehabilitation: Continuous Passive Motion (CPM) mode and master-slave mode. CPM exercise helps restore motor function and proprioception that are lost due to impairment.18-20 During the master-slave mode where the motions of the normal fingers are duplicated to the affected fingers, the device induces active participation of the patient and helps neuroplasticity.
We also suggest two methods to quantitatively evaluate spasticity. First, we estimate spasticity level of patient's finger by fusion of pressure and angle data during CPM. Second, Electromyography (EMG) is used to determine the level of finger extensor muscle activation and to compare passive rehabilitation with active rehabilitation using an air pocket glove.
2. Methodology
2.1 Air Pocket Glove and Control System
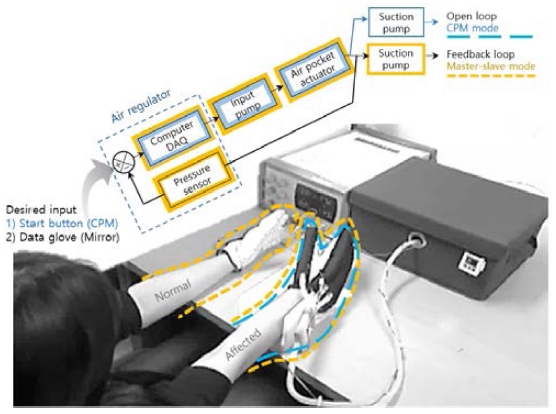
The air pocket glove rehabilitation system is divided into a mechanical and a control part. The device, 86 g in total, consists of a light glove, air pocket-type actuators, silicone flexors and a bending sensor. Each finger contains an actuator and a bending sensor that measures the angle of the paralyzed finger. Additionally, silicone flexors are attached to guide a return path during grasping movement. The control unit consists of two pump motors for injection and discharging the air, solenoid valves (10 channels) for distributing the air, an air regulator for restricting the pressure, and finally a digital pressure sensor for measuring the internal pressure of the actuator.
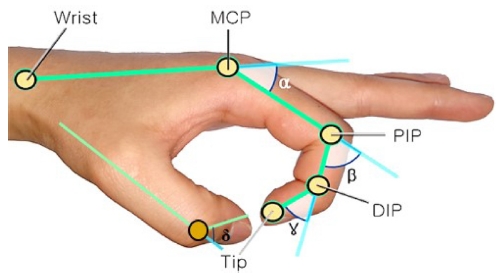
2.2 Air Pocket-Type Actuator
The pneumatic actuator is inflated when air is injected and thus stretches fingers out to extension position. The actuator consists of TPU film, poly fabric, and an air injection cap. TPU is light and flexible material of 0.2 g per 10 mm2. The poly fabric has low elongation and limits the actuator expansion to prevent bursting. It also reduces friction. The internal volume of the fabricated actuator is 55 ml. When air is injected into the actuator, the finger unfolding order is the MCP-PIP-DIP. According to Pascal's principle, the air is not concentrated in one part of the actuator but is evenly distributed to implement the extension motion.
2.3 Silicone Flexor
The silicone flexors are attached to the palm of the air pocket glove to guide finger flexion by elasticity of the silicone for those who cannot grasp. In addition, the silicone flexor acts as a dash pot that improves safety by its spring force applied to each finger joint during extension exercise. The position of the silicone flexor is determined by considering movement around the scaphoid tubercle when a person actually bends the finger.21
In this study, the selected silicone hardness is less than 5A (shore hardness) and the elongation was 700% or less. Table 1 is a characteristic of silicone flexor manufactured by Dragon Skin® and Ecoflex® silicone (Smooth-On, Inc.). As a result of application to patients, silicone less than 00-30 (shore hardness) was not suitable for application due to durability and elongation problem. Therefore, flexors are fabricated with 2A silicone.
2.4 Pneumatic Control System
The rehabilitation system is soft and light due to pneumatic actuators. It also implements slow and precise movement similar to rehabilitation by therapist. The pneumatic system consists of a solenoid valve (12 V, 10 channels), two air pump motors (Motor Bank, Inc., 24 VDC, Rated current: 2A, Max pressure: 600 kPa), a pressure sensor (SMC®, ISE-40A). The solenoid valve receives the feedback from the pressure sensor and the bending sensor attached on the glove to control the air flow direction. The air pump injects constant air into the actuator through voltage control. The air regulator automatically discharges air if the actuator internal pressure exceeds a certain pressure level.
2.5 Air Pocket Glove Characteristics
We performed a test to determine safety and durability of the actuator before applying it to patient. After wearing the air pocket glove, the maximum air pressure limit was determined. Experimental conditions were as follows: After wearing the glove, air was slowly injected into actuator using a piston while finger angles and actuator pressure were monitored. The maximum pressure of the actuator measured through the above procedure is 68.6 kPa. The limit of the air regulator is determined based on the maximum pressure. When the finger reaches certain angle, the solenoid valve is closed to keep the pressure level constant. Table 2 shows the internal pressure according to angle. The angle of the finger is measured between PIP and DIP based on the anthropometric method.22 Therefore, the finger angle decreases with increasing pressure. In addition, the maximum extension is shown at index finger 10o/ 64.4 kPa and thumb 10o/ 68.6 kPa. The reason for the difference between the thumb and the index finger is due to the structural characteristics of the finger, RoM and internal volume (index: 55 mL, thumb: 42 mL). In the master-slave mode, patient's own intent is included and can participate in his rehabilitation. In this mode, the EMG energy level is measured during exercise.
3. Finger Rehabilitation System
3.1 Continuous Passive Motion (CPM) Mode
The CPM mode is aimed at patients’ adaptation to the Air Pocket Glove as well as muscular and joint spasticity relaxation. According to Hesse et al.,23 Periodic and repetitive passive exercise improved the extremity sensation and reduced the Modified Ashworth Scale (MAS) scores of the hemiplegic patients.24 Based on previous studies, the present study designed an effective passive motion, as follows. The CPM exercise is repeated for 20 minutes with a set of 6 seconds of air injection, 3 seconds of holding, and 4 seconds of discharge.
3.2 Master–Slave Mode
In master-slave mode, we applied Mirror Therapy (MT), which is a rehabilitation technique to activate neuroplasticity by imagining unaffected side hand movements as affected side moves. Human’s mirror neurons are bimodal visuomotor neurons that are active during action observation, mental stimulation (imagery), and action execution.25 According to Yavuzer et al.,26 Stroke patients’ hand function was improved after mirror treatment.
In master-slave mode, healthy fingers with a data glove act as a master system whereas affected fingers with the air pocket glove as a slave system. A bending sensor attached to each finger measures the angle of finger joint (MCP to PIP). The sensor on the healthy side acts as a switch depending on the finger angle and controls the solenoid valve and the air motor. Master-slave mode should minimize the time delay between unaffected and normal sides so that the brain simultaneously recognizes both optic and motor nerve stimulation.27-29 Thus, a suction pump was added to the air outlet. As a result, the air discharge time of 42% (5.6 to 2.4 sec) was shortened to allow the patient to perceive the same motion.
4. Result and Discussion
The subject is a left side hemiplegic patient and a brunnstrom stage 3rd - 4th (estimated by physical therapist). This patient is capable of voluntary exercise using orthosis, resistance is stronger at the end of the finger movement during physical therapy. The patient had a MAS score of 1 and a BBT score of 39. The experiment was performed at the Pohang rehabilitation hospital.
4.1 CPM Mode Analysis
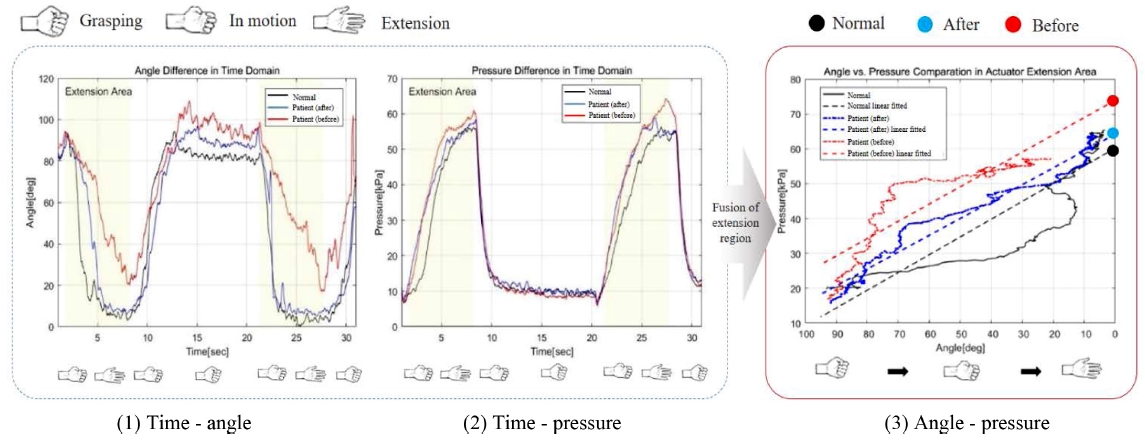
In CPM mode, three cases were compared: 1) normal hand, 2) hand before rehabilitation, and 3) after rehabilitation.
The angle-time graph of the normal hand shows that it reaches 0 to 20o in 3.7 seconds immediately after the pneumatic pressure is applied. In addition, the pressure in the pressure-time graph starts to rise from 2 seconds and rises slowly (4.4 sec) in all three cases. Before rehabilitation, the patient's graph is shown to take 7.8 seconds to reach 0 to 20o. In addition, it can be confirmed that the finger is extended only up to 20o. There is angle difference between the normal hand and the before rehabilitation about 13 deg. Above results indicate that the device has a potential to diagnose spasticity according to the RoM of a patient's finger.
In the case of pressure data, it takes 3.6 seconds to reach 40 kPa and tends to rise the fastest. The highest pressure is 61 kPa. After rehabilitation case took 5 seconds to reach 0 to 20o, and the max angle is 7o In the CPM mode, the inside pressure of the actuator and the patient's finger angle information are determined to confirm the correlation with the patient’s spasticity level. Table 3 shows the lowest pressure value (55 kPa) for the normal hand and the highest pressure value (61 kPa) for the affected hand before rehabilitation. This is because the patient's fingers act as springs trying to return to their neutral positions due to spasticity thus increasing the air pressure inside the actuator. Thus, the pressure data can be used to determine the resistance level of the patient to exercises, and a spasticity level can be estimated based on the resistance level.
Finally, the angle-pressure graph is modelled with linear fitting. A modeled spasticity Eq. (1) is expressed as follows:
| P: pressure, θ: MCP to PIP anglePatient (before): P= -0.4961 × θ+73.93Patient (after): P= -0.4836 × θ+64.22Normal hand: P= -0.5095 × θ+60.22 | (1) |
In the angle-pressure graph in Fig. 5(3), the y-intercept (Eq. (1)) difference between the normal hand and the before rehabilitation hand was 21.1% (before rehabilitation > normal hand). Y-intercept difference between normal and after rehabilitation is measured as 6.6%. At last, the y-intercept value before and after rehabilitation shows a difference of 15.1%. The higher the spasticity level of the subjects, the greater the y-intercept difference. This result shows that the stroke patient’s spasticity level can be diagnosed according to the correlation between the measured angle and pressure using the air pocket glove.
4.2 Master–Slave Mode Analysis
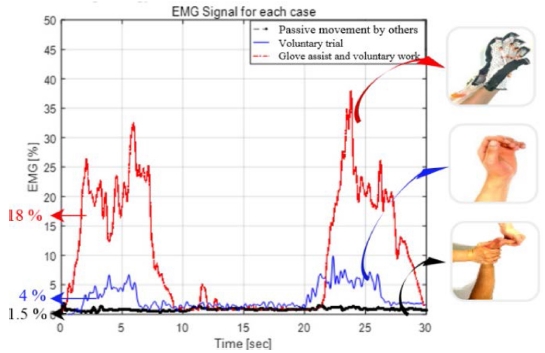
Existing research insists that significant sEMG experiment results are obtained when using a mirror instruction video to perform an affected hand exercise.30 In this study, higher EMG is expected to be measured because not only visual feedback of the hand is included but also the actual motion of the affected hand is exercised. EMG signals were collected during master-slave exercise to analyze any muscle activations according to different conditions of the subject. The EMG energy, expressed in percentage unit, is normalized to the maximum force of the normal hand. Therefore, the y-axis in Fig. 4 indicates how much energy is exerted compared to the normal hands. Conditions were 1) passive movement done by others, 2) voluntary extension (no actual movement), 3) glove-assisted and voluntary extension (actual movement). A pair of EMG electrodes were attached to extensor digitorum muscle (EDM) of the forearm, and a ground was attached to an abdomen. The control procedure of the third condition was injection (8 seconds), discharge (3 seconds), and waiting (3 seconds) using his own hands. We processed the EMG signals using quasi-tension filter proposed by Yasuharu Koike et al..31
| LPF=36.84S2+27.32S+178.4 | (2) |
The passive movement (0 - 8 sec, 20 - 28 sec) shows no change in the EMG energy measured up to 1 - 1.5%. In the second case which is the voluntary trial (no actual movement), EMG energy was measured at an average of 4%. In the third case, EMG energy was measured at an average of 18%. Thus, the biggest difference between EMG energies during the first and third condition was about 16.5%.
In the master-slave mode, in Fig. 4, the EMG energy levels measured in three states can be used to verify the effectiveness of the air pocket glove. The graph of the passive movement done by others shows that the EMG energy of extensor muscles are hardly measured. Based on the experimental conditions, rehabilitation that does not involve self-intent produces very little muscle activation level (1.5%). This means that, in actual rehabilitation, although passive exercise by the physical therapist helps muscle relaxation, the muscle activation level of the patient is not high. On the other hand, when the user put his effort to move fingers with an aid of the glove, an average level of 18% of EMG energy level was measured. Stroke patients have a relatively high threshold value to generate motion. In order to measure EMG, voluntary exercise is required beyond the threshold value because muscles must be activated by nerve stimulation. The air pocket glove helps the patient to exceed the threshold value, which can’t be passed by the patient, and the patient becomes able to exercise. Therefore, the master-slave mode would provide more effective environment to encourage better rehabilitation.
5. Conclusion
The Air Pocket Glove is a system that allows both rehabilitation and evaluation. It can numerically assess the patient’s condition, motivate and engage high involvement by actively participating in rehabilitation. In addition, since voluntary rehabilitation is possible without the help of a therapist, the independence of the patient can be improved, and time-unlimited rehabilitation and evaluation are possible. This study was conducted based on rehabilitation and MT mechanism of the references. MT exercise increases gripping ability and improves strength of the fingers, and the ROI of the joints is increased in experiments on subacute stroke patients.32,33 Based on the above theoretical backgrounds, the experiment were designed and it is expected to be used appropriately for the rehabilitation and assessment of stroke patients because it shows a similarity with the previous experimental results. However, existing rehabilitation studies are based on delicate experiments based on patients with acute, subacute, and chronic conditions, so future studies will focus on the patient's age, damaged area, and duration to increase reliability.
Acknowledgments
This paper was presented at ISGMA 2017
This work was supported by the National Research Foundation of Korea (NRF) grant funded by the Korea Government (MOE) (No. 2017R1D1A3B03035973).
REFERENCES
-
Nakayama, H., Jørgensen, H. S., Raaschou, H. O., and Olsen, T. S., “Recovery of Upper Extremity Function in Stroke Patients: The Copenhagen Stroke Study,” Archives of Physical Medicine and Rehabilitation, Vol. 75, No. 4, pp. 394-398, 1994.
[https://doi.org/10.1016/0003-9993(94)90161-9]

- Kwakkel, G., Kollen, B., and Lindeman, E., “Understanding the Pattern of Functional Recovery after Stroke: Facts and Theories,” Restorative Neurology and Neuroscience, Vol. 22, Nos. 3-5, pp. 281-299, 2004.
- Schwarz, R. J. and Taylor, C., “The Anatomy and Mechanics of the Human Hand,” Artificial Limbs, Vol. 2, No. 2, pp. 22-35, 1955.
-
Hartman-Maeir, A., Soroker, N., Ring, H., Avni, N., and Katz, N., “Activities, Participation and Satisfaction One-Year Post Stroke,” Disability and Rehabilitation, Vol. 29, No. 7, pp. 559-566, 2007.
[https://doi.org/10.1080/09638280600924996]

-
Hartman-Maeir, A., Eliad, Y., Kizoni, R., Nahaloni, I., Kelberman, H., et al., “Evaluation of a Long-Term Community Based Rehabilitation Program for Adult Stroke Survivors,” NeuroRehabilitation, Vol. 22, No. 4, pp. 295-301, 2007.
[https://doi.org/10.3233/NRE-2007-22407]

- Desrosiers, J., Bravo, G., Hébert, R., Dutil, É., and Mercier, L., “Validation of the Box and Block Test as a Measure of Dexterity of Elderly People: Reliability, Validity, and Norms Studies,” Archives of Physical Medicine and Rehabilitation, Vol. 75, No. 7, pp. 751-755, 1994.
-
Mathiowetz, V., Volland, G., Kashman, N., and Weber, K., “Adult Norms for the Box and Block Test of Manual Dexterity,” American Journal of Occupational Therapy, Vol. 39, No. 6, pp. 386-391, 1985.
[https://doi.org/10.5014/ajot.39.6.386]

- Wood-Dauphinee, S., Opzoomer, M., Williams, J., Marchand, B., and Spitzer, W., “Assessment of Global Function: The Reintegration to Normal Living Index,” Archives of Physical Medicine and Rehabilitation, Vol. 69, No. 8, pp. 583-590, 1988.
-
Edwards, D. F., Hahn, M., Baum, C., and Dromerick, A. W., “The Impact of Mild Stroke on Meaningful Activity and Life Satisfaction,” Journal of Stroke and Cerebrovascular Diseases, Vol. 15, No. 4, pp. 151-157, 2006.
[https://doi.org/10.1016/j.jstrokecerebrovasdis.2006.04.001]

-
Mehrholz, J. and Pohl, M., “Electromechanical-Assisted Gait Training after Stroke: A Systematic Review Comparing End-Effector and Exoskeleton Devices,” Journal of Rehabilitation Medicine, Vol. 44, No. 3, pp. 193-199, 2012.
[https://doi.org/10.2340/16501977-0943]

-
Chang, W. H. and Kim, Y.-H., “Robot-Assisted Therapy in Stroke Rehabilitation,” Journal of Stroke, Vol. 15, No. 3, p. 174, 2013.
[https://doi.org/10.5853/jos.2013.15.3.174]

-
Rodgers, H., Shaw, L., Bosomworth, H., Aird, L., Alvarado, N., et al., “Robot Assisted Training for the Upper Limb After Stroke (RATULS): Study Protocol for a Randomised Controlled Trial,” Trials, Vol. 18, No. 1, pp. 340-355, 2017.
[https://doi.org/10.1186/s13063-017-2083-4]

-
Volpe, B. T., Lynch, D., Rykman-Berland, A., Ferraro, M., Galgano, M., et al., “Intensive Sensorimotor Arm Training Mediated by Therapist or Robot Improves Hemiparesis in Patients with Chronic Stroke,” Neurorehabilitation and Neural Repair, Vol. 22, No. 3, pp. 305-310, 2008.
[https://doi.org/10.1177/1545968307311102]

-
Wressle, E., Eeg-Olofsson, A.-M., Marcusson, J., and Henriksson, C., “Improved Client Participation in the Rehabilitation Process using a Client-Centred Goal Formulation Structure,” Journal of Rehabilitation Medicine, Vol. 34, No. 1, pp. 5-11, 2002.
[https://doi.org/10.1080/165019702317242640]

-
Lodha, N., Patten, C., Coombes, S. A., and Cauraugh, J. H., “Bimanual Force Control Strategies in Chronic Stroke: Finger Extension Versus Power Grip,” Neuropsychologia, Vol. 50, No. 11, pp. 2536-2545, 2012.
[https://doi.org/10.1016/j.neuropsychologia.2012.06.025]

-
Fritz, S. L., Light, K. E., Patterson, T. S., Behrman, A. L., and Davis, S. B., “Active Finger Extension Predicts Outcomes after Constraint-Induced Movement Therapy for Individuals with Hemiparesis after Stroke,” Stroke, Vol. 36, No. 6, pp. 1172-1177, 2005.
[https://doi.org/10.1161/01.STR.0000165922.96430.d0]

-
Koo, I., Kang, B. B., and Cho, K.-J., “Development of Hand Exoskeleton Using Pneumatic Artificial Muscle Combined with Linkage,” Journal of the Korean Society for Precision Engineering, Vol. 30, No. 11, pp. 1217-1224, 2013.
[https://doi.org/10.7736/KSPE.2013.30.11.1217]

-
Lin, P. Y., Chen, J. J. J., and Lin, S. I., “The Cortical Control of Cycling Exercise in Stroke Patients: An Fnirs Study,” Human Brain Mapping, Vol. 34, No. 10, pp. 2381-2390, 2013.
[https://doi.org/10.1002/hbm.22072]

-
Takeuchi, N., and Izumi, S.-I., “Rehabilitation with Poststroke Motor Recovery: A Review with a Focus on Neural Plasticity,” Stroke Research and Treatment, pp. 1-13., 2013.
[https://doi.org/10.1155/2013/128641]

-
Ding, Q., Ying, Z., and Gómez-Pinilla, F., “Exercise Influences Hippocampal Plasticity by Modulating Brain-Derived Neurotrophic Factor Processing,” Neuroscience, Vol. 192, pp. 773-780, 2011.
[https://doi.org/10.1016/j.neuroscience.2011.06.032]

- Pechlaner, S. and Kerschlaumer, F., “Atlas of Hand Surgery,” Thieme, pp. 31-55, 2011.
-
Buchholz, B., Armstrong, T. J., and Goldstein, S. A., “Anthropometric Data for Describing the Kinematics of the Human Hand,” Ergonomics, Vol. 35, No. 3, pp. 261-273, 1992.
[https://doi.org/10.1080/00140139208967812]

-
Hesse, S., Schulte-Tigges, G., Konrad, M., Bardeleben, A., and Werner, C., “Robot-Assisted Arm Trainer for the Passive and Active Practice of Bilateral Forearm and Wrist Movements in Hemiparetic Subjects1,” Archives of Physical Medicine and Rehabilitation, Vol. 84, No. 6, pp. 915-920, 2003.
[https://doi.org/10.1016/S0003-9993(02)04954-7]

-
Wittenberg, G. F., Chen, R., Ishii, K., Bushara, K. O., Taub, E., et al., “Constraint-Induced Therapy in Stroke: Magnetic-Stimulation Motor Maps and Cerebral Activation,” Neurorehabilitation and Neural Repair, Vol. 17, No. 1, pp. 48-57, 2003.
[https://doi.org/10.1177/0888439002250456]

-
Rosseland, R. B., “Design and Evaluation of an Interactive Music System for Exercise and Physical Activity with Alzheimer’s Patients,” SoundEffects-An Interdisciplinary Journal of Sound and Sound Experience, Vol. 6, No. 1, pp. 4-22, 2016.
[https://doi.org/10.7146/se.v6i1.24910]

-
Yavuzer, G., Selles, R., Sezer, N., Sütbeyaz, S., Bussmann, J. B., et al., “Mirror Therapy Improves Hand Function in Subacute Stroke: A Randomized Controlled Trial,” Archives of Physical Medicine and Rehabilitation, Vol. 89, No. 3, pp. 393-398, 2008.
[https://doi.org/10.1016/j.apmr.2007.08.162]

-
Summers, J. J., Kagerer, F. A., Garry, M. I., Hiraga, C. Y., Loftus, A., et al., “Bilateral and Unilateral Movement Training on Upper Limb Function in Chronic Stroke Patients: A TMS Study,” Journal of the Neurological Sciences, Vol. 252, No. 1, pp. 76-82, 2007.
[https://doi.org/10.1016/j.jns.2006.10.011]

-
Rothgangel, A. S., Braun, S. M., Beurskens, A. J., Seitz, R. J., and Wade, D. T., “The Clinical Aspects of Mirror Therapy in Rehabilitation: A Systematic Review of the Literature,” International Journal of Rehabilitation Research, Vol. 34, No. 1, pp. 1-13, 2011.
[https://doi.org/10.1097/MRR.0b013e3283441e98]

-
Michielsen, M. E., Selles, R. W., van der Geest, J. N., Eckhardt, M., Yavuzer, G., et al., “Motor Recovery and Cortical Reorganization After Mirror Therapy in Chronic Stroke Patients: A Phase II Randomized Controlled Trial,” Neurorehabilitation and Neural Repair, Vol. 25, No. 3, pp. 223-233, 2011.
[https://doi.org/10.1177/1545968310385127]

-
Banerji, S., Kuah, C. W. K., Heng, J., and Kong, K. H., “A Physio-Neuro Approach to Accelerate Functional Recovery of Impaired Hand After Stroke,” Procedia Engineering, Vol. 41, pp. 257-263, 2012.
[https://doi.org/10.1016/j.proeng.2012.07.171]

- Kim, J., Sato, M., and Koike, Y., “Human Arm Posture Control Using the Impedance Controllability of the Musculo-Skeletal System Against the Alteration of the Environments,” Transactions on Control, Automation, and Systems Engineering, Vol. 4, No. 1, pp. 43-48, 2002.
-
Arya, K. N., Pandian, S., and Kumar, D., “Task-Based Mirror Therapy Enhances Ipsilesional Motor Functions in Stroke: A Pilot Study,” Journal of Bodywork and Movement Therapies, Vol. 21, No. 2, pp. 334-341, 2017.
[https://doi.org/10.1016/j.jbmt.2016.08.001]

- Salem, H. M. A. and Huang, X., “The Effects of Mirror Therapy on Clinical Improvement in Hemiplegic Lower Extremity Rehabilitation in Subjects with Chronic Stroke,” World Academy of Science, Engineering and Technology, International Journal of Medical, Health, Biomedical, Bioengineering and Pharmaceutical Engineering, Vol. 9, No. 2, pp. 163-166, 2015.